Pathological Demand Avoidance (PDA) is a condition associated with Autism Spectrum Disorder (ASD). It is a rare behavioral phenotype of ASD that is characterized by an overwhelming or obsessional need to resist or avoid demands, which can often lead to sensory overwhelm causing meltdowns and violent outbursts.
Although children in general may often try to avoid demands, children with PDA engage in avoidant behaviors at a greater level.
The key underlying factor is the extreme levels of anxiety associated with a loss of control, which can feel like a panic attack. Because of high levels of anxiety, they will often respond with a “No” even to tasks or activities that they normally enjoy and can spend a great deal of energy trying to gain control of situations and people.
(from an Australian PDA article: What is Pathological Demand Avoidance (PDA) and how can we address it? so I changed the spelling of behavioural and characterised to be American)
This is a typical overview of PDA and the common recommendations (as outlined in the above article) are all behavioral interventions: be an active listener and build trust, depersonalize requests, provide indirect praise, use humor and so on. Many parents find these helpful but the biochemical imbalances that trigger these behaviors are being ignored and/or there is a lack of awareness. I’d like to change this so more children and teens get quick relief.
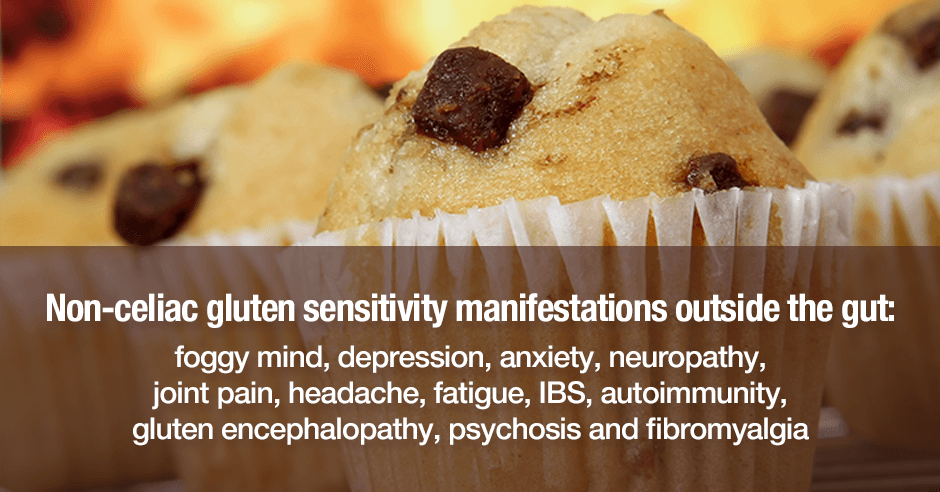
There may be many different root causes such as low serotonin, low GABA, low blood sugar, gluten sensitivities, low zinc, low vitamin B6, low vitamin D, toxins, infections, phenols, salicylates etc. Today I’m going to discuss low serotonin and my rationale for reaching this conclusion. It’s also one of the quickest root causes to confirm (more on that below).
My rationale for proposing that Pathological Demand Avoidance (PDA) in children with autism is related to low serotonin
If we take the description above, all of these symptoms are classically found when a child (or adult) has low serotonin:
- Extreme levels of anxiety
- Can feel like a panic attack
- Overwhelm
- Meltdowns and violent outbursts
- Loss of control
- Spending a great deal of energy trying to gain control of situations and people (i.e. controlling)
- Obsessional need to resist (any kind of obsessing is common when serotonin is low)
The second reason I suspect low serotonin with PDA is the timing of these behaviors i.e. later in the day. The article mentions that “A child with PDA can be very calm, cool and compliant at school and behave much worse at home. This is not because of incompetent parenting but because they have reached their tolerance levels and need to release that suppressed anxiety.”
This may well be a factor, however low serotonin symptoms are recognized as being more severe in the afternoon/evening when serotonin levels start to decline. If these children have low serotonin then it makes sense that these symptoms would start to increase once they get home.
My third reason is that low serotonin is common in autism/autism spectrum disorder (ASD).
Low serotonin is common in autism/autism spectrum disorder (ASD)
This paper, Vitamin D hormone regulates serotonin synthesis. Part 1: relevance for autism, summarizes it as follows: “The disruption of the serotonergic system is one of the most consistent observations associated with autism. Serotonin in the brain promotes prosocial behavior and correct assessment of emotional social cues.”
Their recommendations are vitamin D and tryptophan supplementation which they say “may be a simple method of increasing brain serotonin without negative side effects.”
Testing for low levels of vitamin D and supplementing accordingly is important.
Are there other low serotonin symptoms and using a trial of tryptophan to confirm
As mentioned above, low serotonin is also one of the quickest root causes to confirm. As always, regardless of the diagnosis, we assess for low serotonin by rating symptoms on a scale of 1 to 10 (with 10 being most severe) and do a trial of tryptophan (chewed or a capsule opened on to the tongue). You will have your answer very quickly because we rate improvements in symptoms in the next 5 to 30 minutes.
In addition to the above symptoms we also look for these: worry-in-your-head and ruminating type of anxiety, phobias, lack of confidence, depression, negativity, imposter syndrome, PMS, irritability, insomnia and afternoon/evening cravings for carbs and sugar.
Lidtke is the only brand of tryptophan that I recommend simply because I see it work so well and because of quality issues with tryptophan in the past. Here are the Lidtke tryptophan products I recommend:
- Lidtke Chewable Tryptophan 100 mg is a good for doing a trial and works when lower doses are needed as with children.
- Lidtke Tryptophan 500 mg can be used for doing a trial. I open the capsule and use 100mg for a child. Going forward this product is helpful when higher doses are needed, especially at night. When opened it doesn’t taste very good but can be mixed with inositol or even glutamine powder or mashed banana.
You can read more on this blog: Tryptophan for the worry-in-your-head and ruminating type of anxiety, see the full list of low serotonin symptoms here and find the tryptophan products on the supplements blog here.
If you’re new to PDA, the DSM and low serotonin/other biochemical factors
Professor Elizabeth Newson was a developmental psychologist known for her work with children in the autism spectrum. This is her 2003 paper on the topic – Pathological demand avoidance syndrome: a necessary distinction within the pervasive developmental disorders
It’s not part of the DSM-5, the standard classification of mental disorders used by mental health professionals in the United States. This article, A Brief History of Pathological Demand Avoidance, offers a good backstory and shares why families want it to be part of the DSM.
Whether or not it becomes a distinct condition or autism subtype in the DSM, I’d like to see low serotonin (and likely low vitamin D) being recognized as one root cause. And acknowledging that there may be many other biochemical/nutritional approaches that should also be explored.
These symptoms are listed in the above article, in addition to avoidance behaviors, and all could fall into typical low serotonin symptoms:
- verbal and physical aggression when feeling loss of control
- self-injurious behavior
- property destruction
- refusal to participate in self-care such as bathing or brushing teeth (is this depression?)
- inability to attend social events (is this fear and social anxiety?)
- controlling what noises are allowed in a home, such as no music, or only certain music
- inability to allow parents to have friends visit the home (is this also controlling?)
- are often combative with siblings
- issues with food, what to eat, when to eat, who to eat with
- conflict with siblings
As mentioned above we also look into low GABA and low blood sugar (trials of GABA and glutamine will give quick confirmation too), gluten sensitivity, low zinc, low vitamin B6, toxins, infections, phenols, salicylates and so on. Of course, Nutritional and Dietary Intervention for Autism Spectrum Disorder is crucial.
Some success stories and connecting the dots with low serotonin
These two success stories illustrate how successful tryptophan and GABA can be and also how quickly they offer relief:
- Rage, anxiety, cravings & insomnia in 11-year old girl with RAD/reactive attachment disorder: chewable tryptophan turns things around
- Half a crushed GABA Calm for my autistic child: sleep, anxiety and sensorimotor skills (writing, horse riding and swimming) improve
This blog post illustrates similar low serotonin symptoms and end-of-the-day timing in adults with Alzheimer’s – Sundowning in Alzheimer’s and dementia: melatonin/tryptophan for the agitation, restlessness, anxiety, disturbed sleep and aggression. It’s low serotonin that is the cause, regardless of the diagnosis.
This blog illustrates another mechanism for these types of disruptive behaviors: Christmas tree phenols as a trigger for anger, meltdowns, anxiety, hyperactivity, insomnia, aggression, self-injury and autistic symptoms? There is a serotonin connection when there are phenol issues too.
Resources if you are new to using amino acids as supplements
If you are new to using amino acids as supplements, here is the Amino Acids Mood Questionnaire from The Antianxiety Food Solution (you can see all the symptoms of neurotransmitter imbalances, including low GABA, low serotonin and low endorphins).
If you suspect low levels of any of the neurotransmitters and do not yet have my book, The Antianxiety Food Solution – How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings, I highly recommend getting it and reading it before jumping in and using amino acids on your own so you are knowledgeable. And be sure to share it with the practitioner/health team you or your loved one is working with.
There is an entire chapter on the amino acids and they are discussed throughout the book in the sections on gut health, gluten, blood sugar control, sugar cravings, anxiety and mood issues.
The book doesn’t include product names (per the publisher’s request) so this blog, The Antianxiety Food Solution Amino Acid and Pyroluria Supplements, lists the amino acids that I use with my individual clients and those in my group programs. You can find them all in my online store.
If, after reading this blog and my book, you don’t feel comfortable figuring things out on your own (i.e. doing the symptoms questionnaire and respective amino acids trials), a good place to get help is the GABA QuickStart Program (if you have low GABA symptoms too). This is a paid online/virtual group program where you get my guidance and community support.
If you are a practitioner, join us in The Balancing Neurotransmitters: the Fundamentals program. This is also a paid online/virtual program with an opportunity to interact with me and other practitioners who are also using the amino acids.
Have you been told your child may have Pathological Demand Avoidance (PDA)? Have you only been offered behavioral change tools and how have they helped?
Has low serotonin (and other biochemistry imbalances) been discussed too?
What symptoms does your child have and are things worse later in the day?
Has tryptophan helped reduce the above low serotonin symptoms in your child? How much helps and how quickly?
Or do you find 5-HTP works better? If yes, how much helps and how quickly?
What other biochemical changes have helped?
If you’re a practitioner, are you hearing about increased discussion of Pathological Demand Avoidance (PDA) and do you address low serotonin with your clients/patients?
Feel free to post your feedback and questions here in the comments.