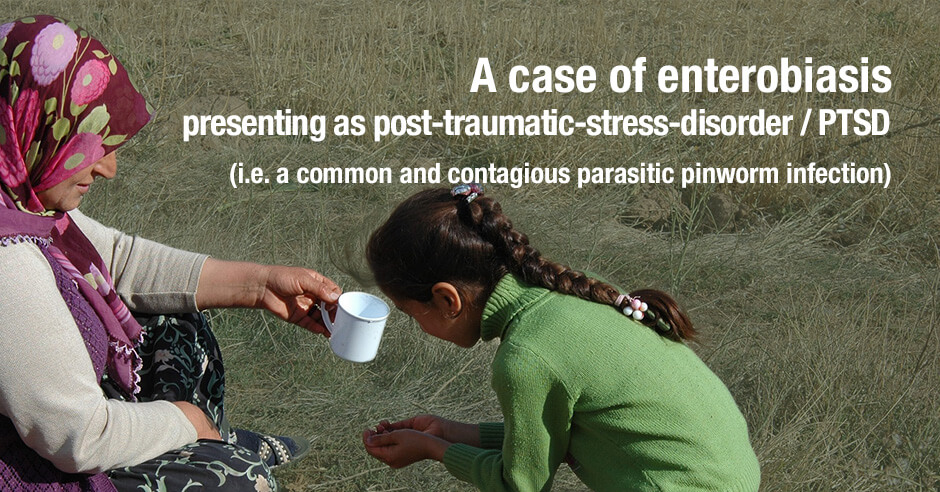
Enterobiasis (oxyuriasis) is a common infection in humans caused by Enterobius vermicularis (E. vermicularis), a human intestinal helminth. Because of the easy way of its transmission among people, it has an extremely high prevalence in overcrowded conditions, such as nurseries and primary schools. Oxyuriasis’s symptoms are extremely diverse in children, ranging from nausea, diarrhea, insomnia, irritability, recurrent cellulitis, loss of appetite, nightmares and endometritis.
Here we report a curious case of oxyuriasis in the settings of a refugee camp in Greece. The patient was a 10-year old Syrian female, who presented with unusual and vague symptoms like insomnia and irritability. Given the violent background of the Syrian warzone that the patient had escaped, she was firstly diagnosed with post traumatic stress disorder (PTSD) before eventually getting correctly diagnosed with enterobiasis.
This infection is the first documented case of enterobiasis in the settings of a refugee camp and can highlight the unsanitary living conditions that refugees have to endure in those camps.
The above is the abstract from a 2017 paper: A case of enterobiasis presenting as post-traumatic-stress-disorder (PTSD): a curious case of the infection with predominant mental health symptoms, presenting for the first time in the settings of a refugee camp
In addition to her symptoms of insomnia and irritability, she had a decreased appetite and mild abdominal (tummy) pain. She was also experiencing nausea and vomiting and had a slightly raised body temperature (subfebrile). She was severely malnourished and had lost 3kg/6.6lbs in 5 days.
Because of the violent nature of her situation she was initially seen by a psychologist but her symptoms worsened in a few days. When this young girl complained about itching in the perianal area (around her anus), the clinic reassessed her and scars around the anal area from the scratches.
They then confirmed enterobiasis/pinworm after using a piece of clear adhesive tape “to collect a specimen from the perianal surface of the girl, for three consecutive mornings … A microscopic examination showed the presence of oval shaped eggs, which is typical for the specific helminth [parasitic worm].”
She was treated with “two doses of albendazole, with each dose two weeks apart, in order to avoid reinfection …. And after a 3 month follow-up period, the patient remains asymptomatic without any signs of recurrence.”
An overview of pinworm infections, symptoms, tape test and treatment approaches
This WebMD article offers an overview of pinworm infections, the symptoms, the tape test and treatment approaches.
As you’ll read it’s not only a problem in refugee camps – it’s “very common in elementary school-aged children” and it’s the most common kind of worm infection in the United States. “Most of the time, pinworm infections don’t cause serious problems.” However, when one child (or adult) gets a pinworm infection it can easily be spread to the entire family. The Syrian refugee paper mentions the whole family was tested.
Systemic infection: female health issues and gut health
The WebMD authors also state, “in rare cases, and especially if you have a lot of them, the pinworms can travel from the anal area up the vagina to the uterus, fallopian tubes, and around the pelvic organs. This can cause inflammation of the vagina (vulvovaginitis).”
I first learned about these serious systemic issues in women from naturopathic doctor Rachel Arthur at a conference in Australia. Contrary to the WedMD article, she believes this is not rare and more common than you’d expect, contributing to hormonal imbalances and even infertility.
The research confirms the impacts of pinworm on the gut, with reports of pinworm associated with appendicitis, pinworm in the liver, pinworms contributing to dysbiosis and pinworm being a factor in inflammatory bowel disease.
The WebMD article doesn’t mention the mental health symptoms and mechanisms but you can read more about that (and my interview with Dr. Jay Davidson) below.
Annual deworming and concerns about drug resistance?
I’m not going to get into anti-parasitic medications and herbal alternatives in this blog post – Dr. Jay talks about mimosa pudica seeds and Dr. Rachel recommends chondroitin sulfate – but do I want to mention that there are many public policy papers calling for annual deworming procedures for everyone. It’s also mentioned in the above Syrian refugee paper, as is hand-washing for prevention.
And many folks recall annual deworming concoctions as a child and did/do the same with their children.
There is, however, the concern about antiparasitic drug resistance similar to what is being seen with antibiotics and antiviral drugs.
If you are new to parasites and their impacts on mood issues, anxiety and insomnia and more
If you are new to parasites, here are some insights from an interview I did with Dr. Jay Davidson on The Anxiety Summit 5: Gut Brain Axis. The topic of our interview is – Parasites, Anxiety and TUDCA for Your Liver. He shares this:
The Greek meaning of parasite is one that sits at another’s table. So essentially think of a parasite as it’s taking things from you. It’s taking nutrients, it’s taking key things that your body needs and literally off of you, not to the point that it’s killing you because then you’re not a good host to give a good environment. So it’s basically just kind of sucking you dry.
We discussed symptoms individuals may experience: mood issues, anxiety and insomnia (especially around full moon). He shared that with insomnia “the big issue that I see is restless sleep where you toss, you turn, you wake often. You can’t just be relaxed when you sleep. Parasites get active when you go to bed. The more active they are within your body and the more you’re trying to calm down, the more your body is getting stressed out. This is where teeth grinding happens when you sleep.
This is very typical and likely the kinds of insomnia symptoms this young refugee girl experienced too. Pinworm is more active at night so the itching around her anus and the need to scratch would have affected her sleep too. This is a classic sign of pinworm.
With regards to anxiety and mood issues and possible mechanisms, Dr. Jay shares how parasites contribute to neurotransmitter imbalances:
Parasites will eat the protein you eat and not allow your body to break down that protein into amino acids. That’s why amino acid therapy can be so beneficial symptomatically and change people’s lives, because they’re getting these amino acids that they’re not getting when they have parasites.
When we digest protein, the amino acids are needed to help us make neurotransmitters. With his amino acid comments, he is making reference to my work with the amino acid tryptophan to support your low serotonin worry-type of anxiety symptoms and the amino acid GABA to support your low GABA physical-anxiety type symptoms. They are wonderful for quick relief of anxiety and mood symptoms, and even help sleep problems too. But as he says “you always want to make sure to go to the underlying cause to remove the parasitic infection.”
Other symptoms of parasitic infection that we discuss at length: restless legs and calf cramping, diarrhea, bowel urgency, SIBO (small intestinal bacterial overgrowth), vertical wrinkles above your mouth, nail-biting, food sensitivities, bed-wetting and night sweats. These are all symptoms that we need to look for and then consider stool testing and/or the sticky tape test/clear adhesive tape test for pinworm (as mentioned in the Syrian refugee paper and WebMD article above).
If you missed this interview and/or summit, you can find the purchase link on the above blog and here.
Tryptophan is not working (possibly because of parasites) and toxoplasma gondii (and GABA/anxiety)
Here is some additional reading on parasites on my site and in the literature:
- Tryptophan doesn’t work, then it does and then it doesn’t: could it be hormonal shifts, dietary factors and/or parasites? As I share here, if you have a very pronounced shift in symptoms for 4-5 days around a full moon each month – more severe insomnia, more anxious, more depressed – I would want to check for parasites (as well as hormonal impacts and everything else covered on this blog).
- Toxoplasma gondii: schizophrenia, bipolar disorder, OCD and unresolved anxiety? As I share in this blog, toxoplasma gondii is a microscopic parasite that infects cats and can be found in the soil – research shows it may be a factor in schizophrenia, bipolar disorder and OCD in susceptible individuals. Could toxoplasma gondii could be one of the root causes of unresolved anxiety? I believe so and feel it’s under-rated.
- In this study, Toxoplasma gondii Infections Alter GABAergic Synapses and Signaling in the Central Nervous System, the authors share that “toxoplasma interferes with GABA signaling in the brain …playing a role in seizures and other neurological complications seen in Toxoplasma-infected individuals.” This particular parasite disrupts the workings of the glutamic acid decarboxylase 67 enzyme (GAD67), used to make GABA from glutamate, and very likely contributes to increased anxiety symptoms too.
Resources if you are new to using tryptophan, GABA and other amino acids as supplements
If you are new to using tryptophan, GABA or any of the other amino acids as supplements, here is the Amino Acids Mood Questionnaire from The Antianxiety Food Solution (you can see all the symptoms of neurotransmitter imbalances, including low GABA and low serotonin).
If you suspect low levels of any of the neurotransmitters and do not yet have my book, The Antianxiety Food Solution – How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings, I highly recommend getting it and reading it before jumping in and using amino acids on your own so you are knowledgeable. And be sure to share it with the practitioner/health team you or your loved one is working with.
There is an entire chapter on the amino acids and they are discussed throughout the book in the sections on gut health, gluten, blood sugar control, sugar cravings, self-medicating with alcohol and more.
The book doesn’t include product names (per the publisher’s request) so this blog, The Antianxiety Food Solution Amino Acid and Pyroluria Supplements, lists the amino acids that I use with my individual clients and those in my group programs. You can find them all in my online store.
If, after reading this blog and my book, you don’t feel comfortable figuring things out on your own (i.e. doing the symptoms questionnaire and respective amino acids trials), a good place to get help is the GABA QuickStart Program (if you have low GABA symptoms). This is a paid online/virtual group program where you get my guidance and community support.
If you are a practitioner, join us in The Balancing Neurotransmitters: the Fundamentals program. This is also a paid online/virtual program with an opportunity to interact with me and other practitioners who are also using the amino acids.
If you or a family member have had a pinworm infection, what symptoms did you experience and was the entire family affected?
Have you had hormonal and/or pelvic issues and/or gut issues as a result of systemic infection with pinworm?
How have other parasitic infections impacted your health?
How familiar are you with the fact that pinworm and other parasites can affect your mood, anxiety and sleep, as well as cause gut issues?
If you’re interested in learning more about testing and herbal protocols please let me know. If you’d like to share what has worked for you please do share too.
If you have other questions and feedback please share them here too.