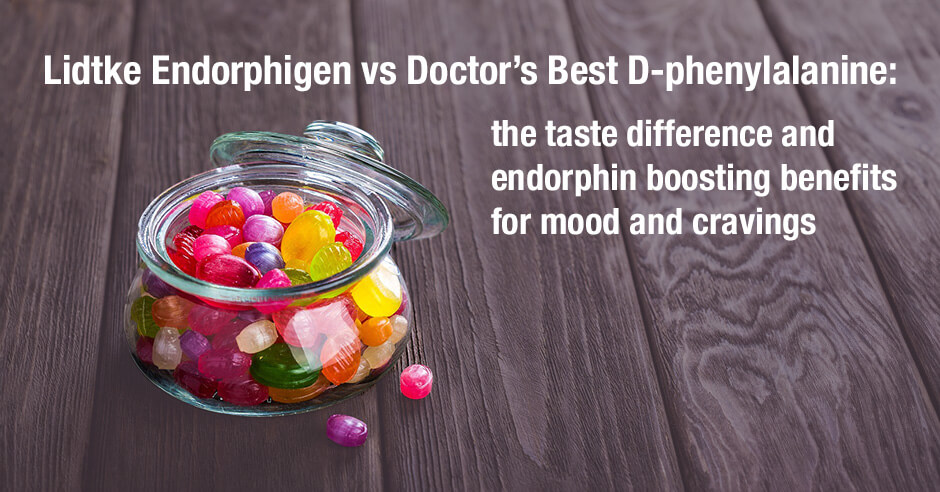
The amino acid d-phenylalanine (DPA) is used to boost endorphins in order to improve mood and reduce cravings. Lidtke Endorphigen has long been a favorite recommendation of mine for this purpose. Doctor’s Best D-phenylalanine is an equally effective and quality product, and both are ideally used opened onto the tongue. When DPA is used this way you get quick results. Many of my clients (and myself included) describe the opened DPA as a dark-chocolate bitter like taste that is not unpleasant. However, about half my clients don’t particularly like the taste of DPA and one woman in my community, Ali, was ready to give up on the Lidtke Endorphigen product because of the taste.
In today’s blog you can read her feedback comparing both products and what worked for her, feedback from a few other women about both products and my personal feedback – with all of us sharing results and taste. And I share some takeaway lessons from these DPA experiences.
She shared this about her strong aversion to the Endorphigen:
Oh goodness. If I open the Endorphigen on my tongue, it’s just awful. I might be able to get 1/4 of it but that’s it. And the taste stays there for at least an hour. No sense of chocolate in there for me. Isn’t that interesting that you and others like the taste. I consider myself pretty open to whatever needs to be done but wow, this is almost no way.
I shared how I love the taste of DPA and that it’s 50:50 in terms of loving it (chocolate-like taste) vs not loving it but also that using the amino acids opened is more effective for many folks. But it’s no good if it tastes bad. I also shared that Lidtke Endorphigen contains a small amount of vitamin B2 and vitamin B6 and maybe that was making it intolerable for her.
Doctor’s Best D-phenylalanine contains DPA only and when I let her know all this, Ali decided to give it a try. This is her feedback on the day she got it:
I received my Doctor’s Best D-phenylalanine and put it on my tongue. It’s 10 bazillion times better than the Endorphigen which was so bad for me that I couldn’t get past it. And I think I can get past a lot. I’m grateful. So now I have to see how it works for me.
Ali’s dark clouds have lifted and her sweet tooth has disappeared
The next day Ali posted this, amazed this product made such a difference in just one day:
I used the Doctor’s Best D-phenylalanine only once and that was today at about 8 am. I felt just generally better, no dark clouds. But also, it’s now 6:30pm when I get my sweet tooth. Nothing. Nothing at all. So no sweet tooth and an improved general feeling. I realize it’s only one day but I feel like it’s made a difference.
And a week later she posted this, confirming that Doctor’s Best D-phenylalanine “is a game changer”:
So much different from Endorphigen. I find I need only 1/2 capsule on my tongue. There’s not much of a taste to me. I then don’t want sweets like I have been wanting in the morning and evening. But I also have a better general feeling. Hard to describe but I just feel more grounded. I can’t tell if it physically reduces the sweet craving or if it’s a mental change. Or both. In any case, nice solid change. Thank you for being there.
Alicia also likes Doctor’s Best D-phenylalanine opened on to her tongue
She shared this about how this DPA product makes her feel:
It gives me a great feeling. Just getting me through some stressful moments. I recommend it! Opening onto the tongue is more effective than swallowing but swallowing adds a bit of relaxation too.
I don’t mind the taste at all – it reminds me of sugar or cocoa powder (my husband was less keen when I got him to try). And it works quickly, yes – I think within 10 minutes but probably less. And I feel more perky for hours. I think I feel more alert but calm emotionally.
I always have a bottle of DPA on hand and I shared my success with Doctor’s Best D-phenylalanine for a recent tooth issue/pain and emotional pain over the holidays on this blog post.
And yet many folks do well with Lidtke Endorphigen and like the taste
I’d like to be clear that this is not intended to be a negative post about Lidtke Endorphigen at all. I still recommend both products and I’ve personally used and like the taste of both. The purpose is to illustrate that we need to find what works for our unique needs and tastes.
As you can see, many folks do really well with the Lidtke product.
Lynn shared this: “I love using the DPA! I use the Lidke brand. Very helpful in improving mood and anxiety. Open on my tongue. I like the taste!”
Joan shared this: “It’s interesting to read your recommendation to open the capsule … I had just started doing that! (Already using powdered forms of other aminos) Anyone looking thru my trash might wonder what I’m up to. This method really works for me.” (she’s using the Lidtke brand).
The addition of vitamin B2 and vitamin B6 to the Lidtke DPA clearly makes no difference in these instances.
The takeaways from this post
- DPA is effective for boosting mood and reducing cravings
- DPA works more effectively when opened on to the tongue and you’ll see results more quickly
- Don’t push through if a product tastes unpleasant
- Don’t give up if one brand doesn’t work for you
- What works for you may not work for someone else
- We all have different taste perceptions – find what works for your unique needs and tastes
- Product formulations change so keep track of exact ingredients on your log and check ingredients when you re-purchase a product
Both DPA products and where to find them
Doctor’s Best D-phenylalanine is available via iherb (use this link to save 5%). Lidtke Endorphigen is available from the company site and from my online store (Fullscript – only available to US customers – use this link to set up an account).
Additional resources when you are new to using DPA and other amino acids as supplements
As a reminder, low endorphins can cause low mood, weepiness, emotional pain, physical pain and emotional eating or cravings. As always, I use the symptoms questionnaire to figure out if low endorphins or other neurotransmitter imbalances may be an issue.
If you suspect low levels of any of the neurotransmitters and do not yet have my book, The Antianxiety Food Solution – How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings, I highly recommend getting it and reading it before jumping in and using amino acids on your own so you are knowledgeable. And be sure to share it with the practitioner/health team you or your loved one is working with.
There is an entire chapter on the amino acids and they are discussed throughout the book in the sections on gut health, gluten, blood sugar control (this is covered in an entire chapter too), sugar cravings, anxiety and mood issues.
The book doesn’t include product names (per the publisher’s request) so this blog, The Antianxiety Food Solution Amino Acid and Pyroluria Supplements, lists the amino acids that I use with my individual clients and those in my group programs (over and above the DPA products I mentioned above).
If, after reading this blog and my book, you don’t feel comfortable figuring things out on your own (i.e. doing the symptoms questionnaire and respective amino acids trials), a good place to get help is the GABA QuickStart Program (if you have low GABA symptoms too). This is a paid online/virtual group program where you get my guidance and community support.
If you are a practitioner, join us in The Balancing Neurotransmitters: the Fundamentals program. This is also a paid online/virtual program with an opportunity to interact with me and other practitioners who are also using the amino acids.
Wrapping up and your feedback
I do always appreciate feedback like this so keep it coming so more folks can get results.
Now I’d love to hear from you – how has DPA helped your mood and cravings (and pain too?)
Which product has worked well for you?
Do you find DPA is more effective if swallowed or as a capsule opened? And how do you describe the taste?
If you’re a practitioner do you use DPA with your clients/patients and have you had this feedback?
And please let me know if it’s helpful that I’m now including product recommendations and where to get them?
Feel free to share and ask your questions below.